Mar 6th, 2024
HIV pre-exposure prophylaxis (PrEP) in Ontario, 2022
Background
HIV pre-exposure prophylaxis (PrEP) is the use of antiretroviral medication on an ongoing basis to reduce one’s risk of acquiring HIV infection. When taken consistently and correctly, PrEP is a highly effective HIV-risk reduction strategy and a critical part of comprehensive HIV prevention. To ensure that everyone who could benefit from PrEP has access to it, it is important to monitor PrEP uptake.
PrEP is recommended for adults who are at risk for acquiring HIV infection through sexual activity or injection drug use. This includes:
- Men who have sex with men (MSM) and transgender women who report condomless anal sex in the last six months who also have at least one other risk factors such as a recent STI, repeated use of post-exposure prophylaxis (PEP), an HIV-positive partner with substantial risk of transmissible HIV or a score of ≥11 on the High-Incidence Risk Index (HIRI)-MSM risk score;
- The HIV-negative partner in heterosexual serodiscordant relationships reporting condomless vaginal or anal sex where the HIV-positive partner is at substantial risk of transmissible HIV;
- People who inject drugs if they share injection drug use paraphernalia with a person with a non-negligible risk of HIV infection.
For more information on the 2017 Canadian guidelines on PrEP use, please see here. Individuals not meeting these strict criteria may also be appropriate for PrEP use based on other considerations and these criteria are not intended to unduly restrict access to this important HIV prevention intervention. As with all health interventions, PrEP prescribing should be individualized and should incorporate health equity and patient preference considerations through joint decision-making with a provider.
Data Sources
Ontario does not currently have a provincial monitoring system for PrEP; the OHTN is able to use pharmacy data on PrEP dispensations to understand PrEP uptake in Ontario between 2018 and 2022. However, there are some important limitations to this data and the ability to assess PrEP uptake. While the data includes some demographic features recorded by the pharmacy, such as age, sex, payer type and geographic location of the pharmacy, there is no information recorded on some very important characteristics (such as race/ethnicity, gender identity, and HIV risk factors). As PrEP uptake should be considered relative to those populations where PrEP is indicated, these data are not adequate to determine whether PrEP uptake has met the need of the key populations at risk for HIV.
Knowledge and awareness of, access to, and targeted uptake campaigns for PrEP are not equal across sociodemographic groups. Understanding the adequacy of PrEP uptake and the equity of distribution will require new data and novel research, supported by community input and guidance.
Methods
The estimated number of PrEP users are based on medication dispensations from a large sample of retail pharmacies across Ontario, which are then projected to the Ontario-level by IQVIA1. This report describes the estimated number, proportion and/or rate of unique individuals dispensed PrEP (known here as “PrEP users”) and describes them overall, by sex, age, prescriber specialty, payer type, region, and as a ratio to the number of first-time HIV diagnoses (“PrEP-to-need ratio”). For the first time in this annual report, we use updated methods to account for online ordering of PrEP, which is then mailed throughout the province and allows for a more accurate description of PrEP dispensation by Ontario geographic region and Public Health Unit (PHU). Furthermore, for the first time, the rate of PrEP dispensation by PHU is reported. The PrEP-to-need ratio by PHU is not reported due to small PrEP dispensation and/or first-time HIV diagnosis counts in some PHUs.
For more information about the blogpost or report, email [email protected]. To learn more about PrEP and how to access it regardless of drug coverage, visit www.ontarioprep.ca.
Some key findings:
PrEP use continues to increase
The estimated number of individuals dispensed PrEP at least once in a calendar period in Ontario has increased year after year; reaching its highest level in 2022 (14,650).

Most PrEP users are men

The majority of PrEP users are male (97.0%), and uptake has been increasing slightly faster among males. Gay, bisexual and other men who have sex with men with certain risk factors make up a large proportion of those for whom PrEP is recommended.
Note: Clinical criteria for recommending PrEP in cisgender women in high income settings such as Ontario are less well developed, and more research is needed to guide its appropriate use. Women who face systemic and social inequities, who are more likely to be exposed to HIV through a sexual or drug injecting partner, require an individualized approach to assess the need for PrEP. Furthermore, these data do not provide adequate insight into whether PrEP is being accessed by other populations at risk for HIV, including heterosexual males and people who inject drugs.
The largest group of PrEP users are between the ages of 30-39.

People get PrEP from their family doctors more than other categories of providers and use private insurance to pay for it
In 2022,
37%
of the estimated PrEP users were prescribed PrEP by a family or general practitioner.
76%
of the estimated PrEP users covered the cost of the prescription through their private health insurance.
PrEP use up in all regions in Ontario
Between 2018 and 2022, the number of PrEP users increased in all regions in Ontario.
The greatest relative increases in PrEP dispensations between 2018 and 2022 were in the Eastern, Central east and Toronto (not Downtown) regions (2.7 times), followed by Ottawa (2.3 times) and Toronto – Downtown (2.2 times).

Most PrEP users are dispensed PrEP in Toronto and Ottawa

Toronto and Ottawa continue to have the largest number of individuals dispensed PrEP. Although they make up 27.0%
of Ontario’s population, together they account for 75.4% of PrEP dispensations in 2022. The concentration of PrEP users in these regions may be explained by Toronto and Ottawa having a higher number of gay, bisexual, and other men who have sex with men (GBMSM) who are eligible for PrEP, physicians and/or clinics that have more experience assessing PrEP appropriateness and/or individuals traveling into these cities to obtain PrEP.
PrEP-to-need ratio
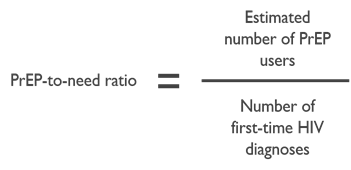
The number of PrEP dispensations alone does not inform whether PrEP uptake is meeting the needs of the province and communities. It is necessary to evaluate PrEP uptake relative to HIV risk. We use first-time diagnoses as a proxy for HIV infection and the risk experienced by the community. Therefore, we examine PrEP use relative to first-time diagnoses, known as the “PrEP-to-need” ratio. The higher the ratio, the closer PrEP use is to meeting the need. We can compare across groups and geographies to understand PrEP uptake relative to need.
However, there are limitations to the interpretation of the PrEP-to-need ratio. First, there is no known cut-off at which we can say PrEP use is at an ideal level and providing optimal community-wide level HIV prevention. Second, it doesn’t assess PrEP appropriateness or eligibility– that is, people taking PrEP in correspondence with clinical guidelines – because we don’t have access to risk information for those on PrEP. Based on insight from community and clinicians, we believe that a large percentage of male PrEP users are gay, bisexual and other men who have sex with men. A first-time diagnosis is not the same as a new HIV infection. Many people living with HIV are not diagnosed in the same year they become infected, and some may have been infected elsewhere and been diagnosed in Ontario. This could overestimate the number of first-time diagnoses, affecting the PrEP-to-need ratio. Lastly, PrEP-to-need ratios at the PHU level are too unstable to report due to small numbers of dispensations and/or first-time diagnoses in some health units.
Note: The number of first-time diagnoses can be influenced by multiple factors, and it is likely to vary by region and population. The numbers should be interpreted with caution.
PrEP use is increasing relative to those who need it in some Ontario regions

Over time, the PrEP-to-need ratio:
- Has increased for both males and females between 2018 and 2022;
- Was higher for males (31.6 in 2022) than for females (2.4 in 2022) but was increasing at a similar pace between 2018 and 2022;
- PrEP-to-need ratio was highest in Toronto and Ottawa, despite a decrease in both regions compared to 2021.
- The decrease from 2021 to 2022 in both Toronto and Ottawa regions is a function of a smaller increase in the PrEP dispensations and a faster increase in first-time diagnoses
For the first time, we are sharing PrEP dispensation information on a Public Health Unit (PHU) level:
- This data allows for the better understanding of PrEP use within smaller Ontario geographic regions. Larger urban areas such as Toronto and Ottawa may have more individuals who are eligible to take PrEP and/or clinicians who are comfortable prescribing PrEP, as well as a higher rate of HIV testing and diagnoses, all which can affect the dispensation rate.
- The highest rate of individuals dispensed PrEP per 100,000 people was in the City of Toronto Health Unit (299.1 per 100,000 people), followed by the City of Ottawa Health Unit (159.3 per 100,000 people) and the City of Hamilton Health Unit (84.1 per 100,000 people).
- The lowest rate of PrEP dispensations were seen in the Porcupine Health Unit (8.0 per 100,000 people), Lambton Health Unit (8.1 per 100,000 people) and Hastings and Prince Edward Counties Health Unit (13.5 per 100,000 people).
- Given the different population demographics in different PHUs, it is anticipated that some areas (e.g. urban areas with a higher number of GBMSM) would have a higher dispensation
Estimated rate of individuals dispensed PrEP per 100,000 people by PHU, 2022

Much more information is provided in the full report.
Footnotes:
- IQVIA, formerly Quintiles and IMS Health, Inc., is an American multinational company serving the combined industries of health information technology and clinical research







